Prostatitis is inflammation of the tissue of the prostate gland in men, which is manifested by pain in the lower abdomen and urination disorders. The disease proceeds in acute and chronic forms, develops under the influence of infectious and non -infectious causes. Prostatitis is included in the five most frequent problems that men turn to the urologist.
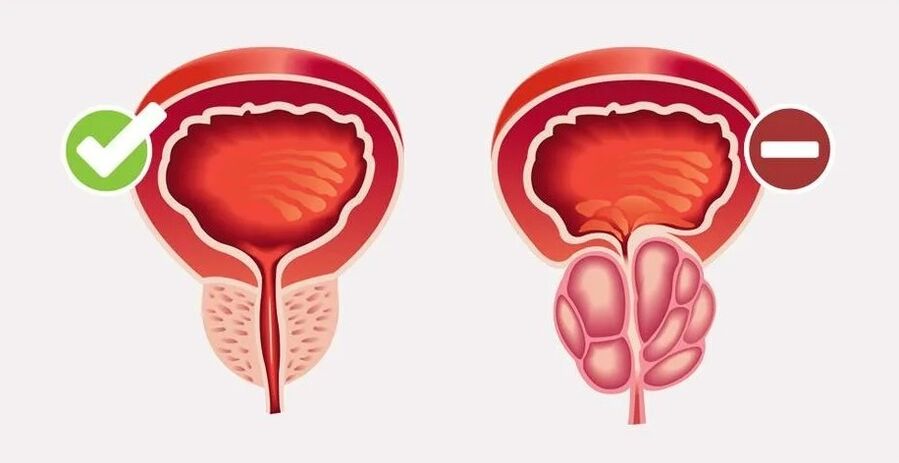
The prostate gland is an organ of the male reproductive system that produces a liquid secret that is part of the sperm and improves sperm mobility. The prostate has the shape of chestnut, dimensions 2x3x3. 5 cm, is located in the middle of the pelvis cavity. A neck of the bladder and the initial department of the urethra pass through the center of the gland.
Acute prostatitis is quite rare (5-10 % of cases), but it proceeds is difficult and is a serious danger to male health. Mostly young men are sick with an acute form of inflammation. Chronic prostatitis develops in men most often aged 60-70 years. The disease proceeds with moderately pronounced symptoms, but over time leads to the formation of erectile dysfunction and impaired urination.
The causes and risk factors of prostatitis in men
All causes of prostatitis in men can be divided into two large groups - infectious and non -infectious.
Acute inflammation of the prostate glandMost often it has an infectious origin, this form of the disease is especially common among men under 40 years of age. In the vast majority of cases, it is caused by bacterial flora:
- Enterococci;
- E. coli;
- Klebsiella and proteas;
- gonococcus;
- pale treponema;
- chlamydia;
- Mycobacteria of tuberculosis.
However, the genitourinary or intestinal infection itself leads to inflammation of the prostate gland in 100 % of cases. For the development of bacterial prostatitis, predisposing factors are required, the main of which is systematic microtrauma of the gland. This happens with prostate biopsy, cystoscopies or operations in the pelvis. Other risk factors of infectious prostatitis include:
- immunodeficiency (HIV infection, congenital pathology of the immune system);
- random sex life;
- homosexual contacts;
- chronic diarrhea or constipation;
- obesity;
- A sedentary lifestyle.
Pathogenic microorganisms penetrate the prostate gland from the urethra or rectum. The weakening of immune protection and microtrauma of the prostate contribute to the development of acute inflammation. Against this background, the tone of the smooth muscles of the prostate rises, which leads to compression of the urethra and urination disorders.
Chronic prostatitisIt has a non -infectious origin and a more complex mechanism of development. Inflammation is formed gradually, and the exact cause of its occurrence has not been established. Risk factors of chronic non -bacterial prostatitis:
- increased pressure in the prostate gland (with benign hyperplasia or adenoma);
- increased pressure in the pelvic cavity;
- chronic pelvic pains;
- autoimmune diseases;
- rare sexual contacts;
- heavy physical activity;
- Chronic stress.
The pathogenesis of chronic prostatitis is based on the stagnation of the secret of the gland, the deterioration of its blood supply, which leads to constant inflammation.
In approximately 6 % of cases, chronic bacterial prostatitis develops in men. The reason for this is insufficient or incomplete treatment of the acute form of the disease.
Types of prostatitis
Depending on the cause and mechanism of development, four clinicalforms of prostatitis:
- acute bacterial;
- chronic bacterial;
- chronic non -bacterial (chronic pelvic pain syndrome);
- asymptomatic inflammation.
The National American Institute of Health distinguishes 4 types of prostatitis dependingFrom the development stage and clinic:
- I type - acute bacterial inflammation with general and local manifestations;
- II type - chronic bacterial inflammation with periods of remissions and exacerbations;
- IIIA Type - chronic non -bacterial (pathogenic microorganisms have not been detected) inflammation confirmed by the presence of leukocytes in the secret of the prostate or ejaculate;
- IIIV type - non -inflammatory prostatitis, in which there are no pathogenic microorganisms and leukocytes in the secret of the gland;
- IV type - asymptomatic inflammation, which can only be confirmed histologically.
DependingFrom the nature of the pathological processIn the prostate gland, they distinguish:
- catarrhal prostatitis - acute uncomplicated inflammation;
- stagnant, or congestative prostatitis - chronic inflammation associated with the obstruction of the ducts of the gland and the accumulation of a prostatic secret in them;
- Calcule prostatitis - a complication of a chronic form of the disease, accompanied by the formation of stones in the ducts of the gland;
- Granumatous prostatitis is an extremely rare form, which is accompanied by a thickening of the mucous membrane of the gland ducts.
Symptoms of prostatitis in men
The clinical picture of prostatitis in men consists of signs of inflammation of the prostate gland, compression of the neck of the bladder and urethra, as well as the general manifestations of the disease. The severity and combinations of symptoms differ depending on the shape and stage of development of prostatitis.
Common manifestationsDiseases, regardless of the form, serve:
- pain in the lower abdomen, lower back, coccyx and sacrum;
- violation of urination in the form of rapid urge, discomfort and burning, intermittent stream;
- Violation of potency and ejaculation.
The acute form of prostatitis begins suddenly, proceeds with pronounced symptoms, is often accompanied by various complications. Chronic inflammation develops gradually, it is characterized by periods of exacerbations and remissions. With bacterial prostatitis, the first symptoms are signs of general intoxication (fever, nausea), and with a non -infectious form of the disease, local inflammation of the prostate is of the main importance.
Signs of acute prostatitis
With acute bacterial inflammation of the prostate, the following symptoms appear in men:
- general malaise;
- fever of more than 38 ° C;
- nausea and vomiting;
- severe pain in the lower abdomen with radiation in the rectum;
- frequent, but at the same time difficult urination;
- itching and burning in the urethra;
- clouding of urine, the appearance of blood or pus in it.
In the future, a complete recovery occurs against the background of treatment, or the chronic form of bacterial prostatitis with various consequences develops.
Symptoms of chronic prostatitis
When forming chronic bacterial prostatitis after acute inflammation, a man is worried about periodic pains in the lower abdomen, difficulty urination, sometimes burning in the urethra. The pain can also spread to the lower back and coccyx, to the rectum, the penis and scrotum. Symptoms usually occur during the period of exacerbation of prostatitis, and during remission, the well -being of a man remains normal.
Non -infectious prostatitis in men is also called chronic pelvic pain, which includes both pain and signs of urination and sexual disorders. It is difficult for a man to urinate, since a stream of urine is sluggish and intermittent, there is a burning sensation and a sense of pressure in the urethra. With a prolonged course of the disease, potency violation occurs, ejaculation becomes inferior and painful. Ultimately, a man’s quality of life suffers significantly, psychological problems develop.
Pain with prostatitis
Pain syndrome with prostatitis is a constant and most pronounced symptom, which is present in all forms of the disease. The mechanism of pain in prostatitis is due to inflammation and edema of the gland, compression of the receptors in the neck of the bladder and the initial section of the urethra.
The acute form of the disease is accompanied by the most severe pain, since inflammation is infectious, leads to a massive edema of the gland. The pain is localized in the prostate itself, but the man feels it not only in the lower abdomen, but also in the lower back, core, rectum and scrotum.
With chronic inflammation of the prostate, painful pain, but they are longer in nature, may not disappear even during the period of remission. The syndrome of chronic pelvic pain is accompanied by unpleasant sensations primarily in the prostate gland itself, as well as in the tailbone, around the anus, at the base of the penis and scrotum. Discomfort bothers the man daily for at least three months.
Than the prostate inflammation is dangerous
Complications develop both with acute and chronic forms of prostatitis:
- vesiculite (inflammation of the seed bubbles);
- colliculite (inflammation of seed tubercles);
- prostate abscess (abscess in the capsule);
- prostate fibrosis (the formation of scars in the tissue of the gland);
- cysts in the prostate;
- prostate stones;
- infertility due to deterioration in sperm quality;
- erectile dysfunction caused by both chronic pelvic pain and psychological disorders;
- depression.
Diagnosis of inflammation of the prostate gland
When the first signs of prostatitis appear, you need to contact a urologist. First of all, the doctor talks with the patient to determine the nature of complaints and collect an anamnesis. For this, the doctor asks the following questions:
- how long the symptoms of the disease have appeared;
- where the pain is localized, its character and conditions of occurrence;
- Are there any problems with urination and ejaculation;
- Are there any chronic diseases, including genitourinary infections.
To diagnose prostatitis, the doctor uses the following methods:
- finger rectal examination of the prostate gland;
- general clinical blood tests;
- bacteriological examination of ejaculate or prostatic secretion;
- ultrasound examination of the pelvic organs;
- Urofloometry;
- radiography or computed tomography of the prostate;
- In rare cases, a biopsy of the prostate gland may be required, followed by histological examination.
Methods of treatment of prostatitis in men
For the treatment of prostatitis in men, mainly conservative methods are used, tactics depend on the cause and stage of the development of the disease. With asymptomatic inflammation (type IV), active treatment is not required. In other forms of the disease, complex treatment is indicated, the acute form of prostatitis requires hospitalization in the hospital, chronic inflammation can be treated on an outpatient basis.
First of all, the doctor gives recommendations on lifestyle corrections:
- rejection of smoking and drinking alcohol;
- regular sex life;
- exclusion of stress;
- adequate physical activity;
- balanced diet;
- Exception of hypothermia and overheating.
A prerequisite for the successful treatment of prostatitis is Elimination of related diseases, especially urogenital infections.
Drug therapy With prostatitis, it is aimed at suppressing the inflammatory process, improving urination and relief of pain. The following groups of drugs are used:
- Antibiotics. Showed by acute bacterial inflammation, the doctor prescribes drugs taking into account the results of the microbiological examination of the secret of the prostate. Medicines can be taken orally in the form of tablets, or in the form of intramuscular injections. The course of treatment is usually 4-6 weeks with an acute form of the disease. In chronic bacterial prostatitis, the duration of therapy is determined individually.
- Alpha-blockers. The drugs are designed to improve urination, as they relax the smooth muscles of the gland and eliminate the compression of the prostatic of the urethra. In the chronic form of the disease, they must be taken for a long time, and sometimes for life.
- Musorelaxants and non -steroidal anti -inflammatory drugs. They are shown to eliminate the pain syndrome caused by inflammation of the gland and spasm of its muscles.
- In chronic inflammation, drugs for improving microcirculation, immunomodulators, antidepressants, drugs for stimulating erection are indicated.
Acute inflammation of the prostate gland amenable to drug treatment, in most cases, a complete recovery occurs within 1. 5-2 months. In the chronic form of the disease, therapy is carried out for a long time, for several years or for life.
An important way of treating congestive prostatitis is the massage of the prostate gland through the rectum. The procedure is performed by a urologist, on an outpatient basis. Massage helps to remove muscle spasm, stimulates the release of a prostatic secret.
Physiotherapeutic procedures shown in the chronic course of prostatitis:
- laser therapy;
- electrophoresis and ultrafonophoresis;
- microwave therapy;
- electrical stimulation;
- acupuncture.
Surgical intervention It is shown only with the development of complications - an abscess or prostate stones.
Forecast and prevention
The prognosis for recovery in acute bacterial prostatitis is favorable subject to timely and complex treatment. The transition to a chronic form is observed in 6-10 % of cases. Chronic non -bacterial prostatitis, as a rule, cannot be completely cured. Complex therapy allows you to slow down the progression of the disease, preserve the quality of the man’s life and reduce the risk of complications.
Prevention of the development of prostatitis in men includes the following recommendations:
- healthy lifestyle;
- regulation of the regime of work and rest;
- balanced diet and drinking mode;
- adequate physical activity;
- regular sex life (ejaculation);
- prevention of genitourinary infections;
- restriction of invasive manipulations (cystoscopy, catheterization of urethra, prostate biopsy);
- Prevention of genital injuries.















